By James Varney for RealClearInvestigations
Strung out on drugs half her life, Brandi Edwards, 29, said the longest she held a job before getting sober four years ago was “about two and a half months.”
Brandi Edwards, 29: Clean now, but few in her former addict circle have returned to productive life, she says, while most are dead or incarcerated.
“I worked at an AT&T call center, a day-care center for a month, fast food places, but I had to take drugs to get out of bed in the morning and when I did show up, I wasn’t productive,” the West Virginia mother of three told RealClearInvestigations. “The first paycheck came along and I was out of there.”

In jail for the ninth time on drug-related charges, and separated from her children, Edwards had an awakening in “looking hard at what I’d lost.” Now clean for four years after rehab, she is married and back in her children’s lives with a home in Princeton, W. Va., and a steady job.
But such success stories are too infrequent to offset the massive cost of the opioid epidemic to the American workforce. Only a couple of people in her former addict circle have returned to productive life, she says, while most are dead or incarcerated.
That toll on labor, haunting America’s working present and future probably for years -- if not decades -- to come, is largely invisible and underreported because it is difficult to measure, according to physicians, counselors, economists, workers and public officials. But its staying power is suggested by other lasting national challenges, including the porous southern border -- a major conduit for smuggled, Chinese-made fentanyl -- and economic and social traumas set in motion by the coronavirus pandemic.
In addition to untold years of productivity lost from fatal overdoses, the nation’s labor participation rate has shrunk steadily since 2000. Precise correlation is elusive, but any graph of that decline would stand in sharp contrast to the rise of opioid addiction in the U.S. And while it is difficult to calculate just how much drug use has caused absenteeism, tardiness and stretches of disability, the connection is strong, as Brandi Edwards’ experience suggests.
“We’ve been writing about this for years but it doesn’t seem to get a lot of traction,” said Dr. Gary Franklin, a research professor at the University of Washington who served as the medical director of the state’s Department of Labor and Industries. “People have not realized how much opioids contribute to disability and lost productivity, and I don’t know if anyone has been able to put a number on that.”
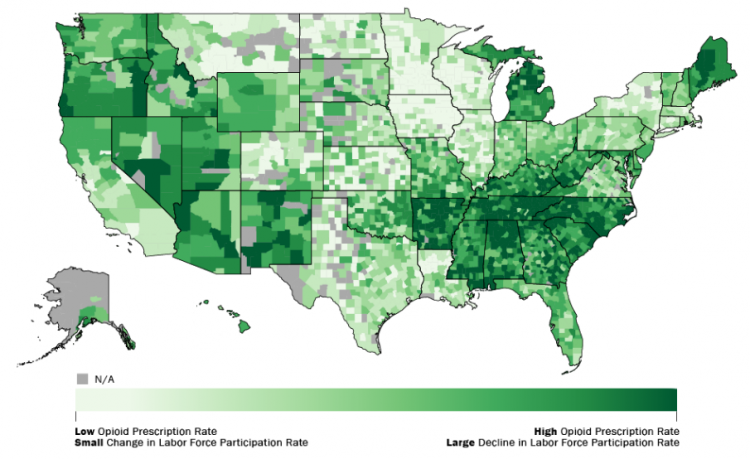
Low workforce participation rates tracked high opioid prescriptions even before the pandemic.
Headline figures on lives lost in the opioid epidemic have been fairly clear for years. In 2021, more than 107,000 people died from drug overdoses, a nearly 15% increase from the year before and more than double the grim tally recorded in 2015, according to the Centers for Disease Control. All told, overdose deaths are seven times higher than they were in 1999.

Synthetic opioids such as fentanyl, which law enforcement has tracked from labs in China along trafficking routes through Mexico on the southern border, are now driving the overdose epidemic. The CDC attributed 69,000 overdose deaths to synthetic opioids in 2020, 82% of the nation's total that year. Heroin overdoses, meanwhile, went up 7% in 2020 to 13,000, according to CDC figures.
That means synthetic opioids and heroin dwarf cocaine and methamphetamines, although totals for both of those have been rising for a decade and often cause overdose deaths in combination with opioids. The National Institutes of Health shows fewer than 5,000 people killed by cocaine alone and fewer than 10,000 by what it dubs "psychostimulants," which includes methamphetamines, in 2020.
Less precisely, economists since at least 2017 have pegged at over $1 trillion the epidemic’s annual dollar cost in terms of deaths, law enforcement and “lost productivity.”
But the amount attributable to deaths - $550 billion of the $1 trillion - is largely conjecture because it is derived from actuarial estimates for lost years; for example, the decades cut from what would have been a normal working life for someone who fatally overdoses at age 45.

Then there is the less lethal side of the equation -- one that workers and employers grapple with daily. Roughly 8% of workplace fatalities in 2020 - 388 of 4,786 - were attributed to "unintentional overdose from nonmedical use of drugs," according to the Bureau of Labor Statistics. However, the agency said it is unclear "how many of these deaths involved opioids specifically."
A post on a neighborhood social media platform asking about opioids’ dire impact in the workforce unleashes a barrage of firsthand horror stories. Homeowners speak of an inability to hire handymen, painters, landscape workers and the like.
“If I’m lucky enough to have an employee that can pass a [urine analysis] the chances of them doing so after the first check is slim,” wrote a tree surgeon in suburban New Orleans. “Tree men get a terrible rap. People think we are all crazy, wild, no fear having, hard working dopeheads.”
But he acknowledged some truth to the stories of workplace abuse of prescription opioids, mentioning laborers’ common habit of relying on increasingly higher-milligram dosages of pain pills like Percocet.
Workers “didn’t wake up one day and say, ‘Hmmm, great day to go down a road that will cost me it all,’ " he wrote. "Then it’s inevitable. We get hurt. Usually pretty badly. So we start out getting a few .5 [mg] maybe 7.5. Later, as our careers go so does the pain, so do the amounts needed to consume to keep it at bay.”
A National Safety Council study reported that more than 75% of U.S. employers have been affected by employees’ prescription drug use, according to congressional testimony, and the National Institutes of Health estimates some 3 million Americans, including workers, are addicted to opioids.
Edwards managed to break her addiction and return to the workforce with the help of Jobs & Hope, a statewide West Virginia placement initiative launched in 2019 that claims more than 1,500 success stories. But with a budget of $3.1 million it cannot handle all of the 200-250 addicts referred to it each month, said Deb Harris, the group’s lead transition agent.
Businesses have been largely receptive to such programs, but the state is still trying to regain its footing from the “flood of pills” that hit it early in the 21st century, according to Dr. Matthew Christiansen, director of West Virginia’s Office of Drug Control in the Department of Health and Human Services.
“We don’t keep a running tally at the state level, but the numbers have probably stayed pretty consistent or maybe gotten a little bit worse because of an increase in overdose deaths due to fentanyl,” Christiansen said.
The Centers for Disease Control does keep a tally, although it hasn’t publicly updated the grim numbers on its “opioid dashboard” since 2017. The figures from that year show that the biggest economic hit has come in the Appalachian states around the Ohio Valley and in New England, two regions where opioids and synthetics have torn a hole through the workforce.
For example, West Virginia, long considered ground zero in the opioid epidemic, had the biggest annual per capita loss due to opioids at $7,247, according to the CDC figures that include overdose deaths. That tops Ohio, where the per capita cost in 2017 was $6,226, and New Hampshire at $5,953. Ohio saw the highest overall economic cost, at $72.58 billion, followed by Massachusetts at $36.91 billion, according to the CDC.
Fixing opioid disorder costs is complicated by the fact much of it is now driven by black-market synthetic drugs like fentanyl and thus can no longer be tracked through prescriptions. Nor is substance abuse a topic that workers - or many employers - are comfortable quantifying. All those involved in coping with the epidemic, however, peg the cost as staggering.
“It’s difficult to measure these things but it’s likely a substantial part of the labor decline,” said Michael Betz, an economist at The Ohio State University who researches opioid disorder issues. “You’re piecing together different pieces of evidence, but when you look at the decline in labor participation rates and opioid disorder figures, they match up pretty similarly.”

Franklin’s team did calculate the odds opioids influenced the disability bills Washington state taxpayers foot each year for roughly 100,000 workers, a relatively uncomplicated tally since Washington is one of four states with a centralized government system and not a private workers’ compensation insurance market.
“We found that two prescriptions of opioids for more than 7 days in the first six weeks after an injury doubled the risk of a worker being on disability one year later,” he said.
Answers to broader questions on opioids’ baleful economic impact, however, are scarce.
“Productivity losses due to anything is an extremely complex analysis and is not routinely tracked,” Franklin said.
To date, the nation's prime age labor workforce has not recovered to where it was at the beginning of 2020 and is now the lowest it has been in 45 years. The hit has been especially pronounced among older adults, according to the Government Accountability Office.
Between 2015 and 2019, adults 50 years old or older "were an estimated 22 percent less likely to be in the labor force (either employed or actively seeking work),” a GAO report found. In addition, people in that age group "were an estimated 40 percent less likely to be employed; and employed older workers who misused opioids were twice as likely to have experienced periods of unemployment."
Once again, however, pinpointing the precise connection between opioids and lost productivity remained elusive, as "the data did not allow GAO to determine causality."
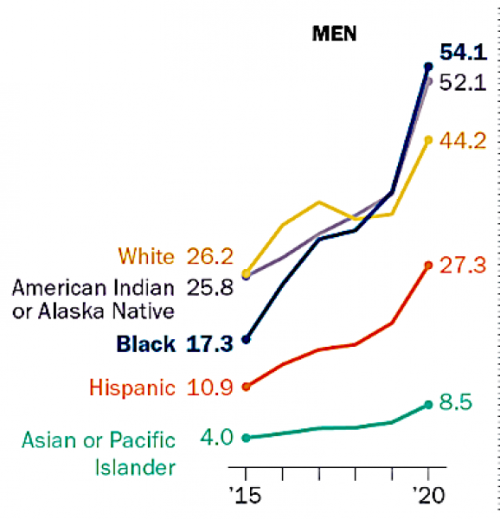
The OD rate for black men recently surpassed that for whites.
Middle-aged white men have long comprised the single biggest group of annual overdose deaths, but between 2015 and 2020 the rate among black men skyrocketed to 54.1 per 100,000, topping white men’s 44.2 per 100,000, according to the Pew Research Center.
“Local economic conditions play some part in all this but they aren’t the key role; the main driver is the increase in supply,” Betz said.
That leads some experts on the topic to conclude that opioids’ catastrophic hit to the United States’ workforce has been misconstrued. For a time, as deaths rose early on, particularly among middle-aged white men, and labor participation rates began their decline, the phrase “deaths of despair” took hold among some researchers.
Under this theory, the opioid epidemic fed on declining economic prospects, particularly for middle-aged white men facing unemployment or shrinking incomes.
But the “deaths of despair” theory reverses cause and effect, according to some physicians and people dealing with the fallout from opioids, including their more deadly synthetic cousin fentanyl.
“We’ve debunked that,” said Dr. Andrew Kolodny, a faculty member at Brandeis University whose practice has specialized in opioid addiction. “Rather than economic conditions leading to overdose deaths it’s really the other way around - it’s not the economy driving them to death, it’s the opioid crisis affecting the economy.”
Link to the original article.